Abstract
Research Article
Dysfunctional breathing in children
Amanda MP Trompenaars#, Aalt PJ Van Roest# and Anja APH Vaessen-Verberne*
Published: 30 May, 2020 | Volume 4 - Issue 1 | Pages: 001-005
Objective: Dysfunctional breathing (DB) refers to abnormal patterns of breathing. No gold standard exists for diagnosis. In clinical practice we regularly see children with functional breathing problems. We collected data from this patient group to gain more insight into the characteristics of children with dysfunctional breathing.
Methods: We composed a retrospective, cross-sectional study. The population consisted of children referred to a physiotherapist by a pediatrician due to suspected dysfunctional breathing. Data from 2013-2015 were collected from patient files, selected according to patterns and onset of symptoms, concomitant asthma, Nijmegen questionnaire (NQ) score, maximum exercise capacity and breathing pattern.
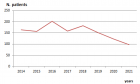
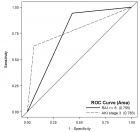
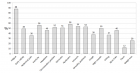
Results: A total of 201 patients were included in the study, 66% of whom were female. The mean age was 13.9 years; 26% of the children were overweight. The most frequently reported symptoms were breathlessness, chest pain/tightness and dizziness. Fifty-two percent had a NQ score ≥23, mainly female. Twenty-eight percent of the children scored < p5 for their age on maximum exercise capacity; this proportion was substantially higher among males. Of the total population, 78% scored < p50 for their age. Subgroups with a higher body mass index (BMI) showed lower maximum exercise capacity. Children presenting with pulmonary symptoms were primarily misdiagnosed with asthma.
Conclusion: Dysfunctional breathing is a common cause of respiratory complaints. Most children with dysfunctional breathing have a high BMI and are in poor physical condition, which suggests a clinically relevant comorbidity and possible options for therapy. Children are often falsely diagnosed with asthma; better recognition will decrease unnecessary medication use.
Introduction
Read Full Article HTML DOI: 10.29328/journal.jprr.1001013 Cite this Article Read Full Article PDF
Keywords:
Hyperventilation; Breathlessness; Asthma; Maximum exercise capacity; Obesity; Nijmegen questionnaire
References
- Barker N, Everard ML. Getting to grips with 'dysfunctional breathing'. Paediatr Respir Rev. 2015; 16: 53-61. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25499573
- Boulding R, Stacey R, Niven R, Fowler SJ. Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev. 2016; 25: 287-294. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27581828
- van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985; 29: 199-206. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4009520
- Thomas M, McKinley RK, Freeman E, Foy C, Price D. The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 2005 14: 78-82. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16701702
- Lear SA, Brozic A, Myers JN, Ignaszewski A. Exercise stress testing. An overview of current guidelines. Sports Med. 1999; 27: 285-312. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10368877
- Stuart RJ, Jr., Ellestad MH. National survey of exercise stress testing facilities. Chest. 1980; 77: 94-97. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7351157
- van der Cammen-van Zijp MH, van den Berg-Emons RJ, Willemsen SP, Stam HJ, Tibboel D, H IJ. Exercise capacity in Dutch children: new reference values for the Bruce treadmill protocol. Scand J Med Sci Sports. 2010; 20: e130-136. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19422656
- Gulmans VA, de Meer K, Binkhorst RA, Helders PJ, Saris WH. Reference values for maximum work capacity in relation to body composition in healthy Dutch children. Eur Respir J. 1997; 10: 94-97. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9032499
- TNO Groeicalculator voor professionals: TNO (toegepast-natuurwetenschappelijk onderzoek); 2010. https://groeiweb.pgdata.nl/calculator.asp
- Stanton AE, Vaughn P, Carter R, Bucknall CE. An observational investigation of dysfunctional breathing and breathing control therapy in a problem asthma clinic. J Asthma. 2008; 45: 758-765. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18972291
- Agache I, Ciobanu C, Paul G, Rogozea L. Dysfunctional breathing phenotype in adults with asthma - incidence and risk factors. Clin Transl Allergy. 2012; 2: 18. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22992302
- Courtney R, van Dixhoorn J, Cohen M. Evaluation of breathing pattern: comparison of a Manual Assessment of Respiratory Motion (MARM) and respiratory induction plethysmography. Appl Psychophysiol Biofeedback. 2008; 33: 91-100. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18320303
- Parreira VF, Vieira DS, Myrrha MA, Pessoa IM, Lage SM, Britto RR. Optoelectronic plethysmography: a review of the literature. Rev Bras Fisioter. 2012; 16: 439-453. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23184278
- Ozgen IT, Cakir E, Torun E, Gules A, Hepokur MN, Cesur Y. Relationship Between Functional Exercise Capacity and Lung Functions in Obese Chidren. J Clin Res Pediatr Endocrinol. 2015; 7: 217-221. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4677557/
- Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med. 2002;162: 1477-1481. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12090884
- Gridina I, Bidat E, Chevallier B, Stheneur C. Prevalence of chronic hyperventilation syndrome in children and teenagers. Arch Pediatr. 2013; 20: 265-268. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23375424
- de Groot EP, Duiverman EJ, Brand PL. Dysfunctional breathing in children with asthma: a rare but relevant comorbidity. Eur Respir J. 2013; 41: 1068-1073. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23018913
Figures:
Figure 1
Similar Articles
-
Fluticasone furoate/Vilanterol 92/22 μg once-a-day vs Beclomethasone dipropionate/Formoterol 100/6 μg b.i.d. in asthma patients: a 12-week pilot studyClaudio Terzano*,Francesca Oriolo. Fluticasone furoate/Vilanterol 92/22 μg once-a-day vs Beclomethasone dipropionate/Formoterol 100/6 μg b.i.d. in asthma patients: a 12-week pilot study . . 2017 doi: 10.29328/journal.jprr.1001004; 1: 013-022
-
Eosinophilic otitis media and eosinophilic asthma: Shared pathophysiology and response to anti-IL5Marieke T Drijver-Messelink*,Mariette Wagenaar,Jacqueline van der Meij,Anneke ten Brinke. Eosinophilic otitis media and eosinophilic asthma: Shared pathophysiology and response to anti-IL5 . . 2019 doi: 10.29328/journal.jprr.1001011; 3: 009-012
-
Dysfunctional breathing in childrenAmanda MP Trompenaars#,Aalt PJ Van Roest#,Anja APH Vaessen-Verberne*. Dysfunctional breathing in children. . 2020 doi: 10.29328/journal.jprr.1001013; 4: 001-005
-
COVID-19 disease with persistently negative RT-PCR test for SARS-CoV-2Sánchez Ríos Carla Paola*, Jiménez Cabrera Oscar Gabriel,Oropeza Lutzow Rebeca,Vázquez Rojas Hazel,Barreto Rodríguez José Omar,Guzmán-Casta Jordi,Guzmán-Huesca Jorge,Riera-Sala Rodrigo,Centeno Sáenz Gustavo Iván. COVID-19 disease with persistently negative RT-PCR test for SARS-CoV-2. . 2020 doi: 10.29328/journal.jprr.1001014; 4: 006-010
-
Spontaneous pneumomediastinum associated with COVID-19: Rare complication of 2020 pandemicArnaldo A Nieves-Ortiz*,Vanessa Fonseca-Ferrer, Kyomara Hernández-Moya,Keren Mendez Ramirez,Jose Ayala-Rivera,Marangely Delgado, Juan Garcia-Puebla,Rosangela Fernández-Medero,Ricardo Fernandez-Gonzalez. Spontaneous pneumomediastinum associated with COVID-19: Rare complication of 2020 pandemic. . 2020 doi: 10.29328/journal.jprr.1001016; 4: 018-020
-
A Case series on Asthma-COPD overlap (ACO) is independent from other chronic obstructive diseases (COPD and Asthma)Divya Khanduja*, Naveen Pandhi. A Case series on Asthma-COPD overlap (ACO) is independent from other chronic obstructive diseases (COPD and Asthma). . 2021 doi: 10.29328/journal.jprr.1001025; 5: 054-058
-
Asthma and pregnancy prevalence in a developing country and their mortality outcomesRaul Aguilar*,Jorge Martinez,Edgar Turcios,Victor Castro. Asthma and pregnancy prevalence in a developing country and their mortality outcomes. . 2021 doi: 10.29328/journal.jprr.1001031; 5: 088-093
-
Spontaneous pneumomediastinum: case reportPedrós García Sergio,Yakasova Elena,Roquet-Jalmar Saus María,Gutiérrez González Nuria,Mercedes Noboa Edwin*. Spontaneous pneumomediastinum: case report. . 2022 doi: 10.29328/journal.jprr.1001034; 6: 001-003
-
Obesity in Patients with Chronic Obstructive Pulmonary Disease as a Separate Clinical PhenotypeDaria A Prokonich*, Tatiana V Saprina, Ekaterina B Bukreeva. Obesity in Patients with Chronic Obstructive Pulmonary Disease as a Separate Clinical Phenotype. . 2024 doi: 10.29328/journal.jprr.1001060; 8: 053-055
Recently Viewed
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Late discover of a traumatic cardiac injury: Case reportBenlafqih C,Bouhdadi H*,Bakkali A,Rhissassi J,Sayah R,Laaroussi M. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019: doi: 10.29328/journal.jccm.1001048; 4: 100-102
-
A two-phase sonographic study among women with infertility who first had normal sonographic findingsKalu Ochie*,Abraham John C. A two-phase sonographic study among women with infertility who first had normal sonographic findings. Clin J Obstet Gynecol. 2022: doi: 10.29328/journal.cjog.1001117; 5: 101-103
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Analysis of Psychological and Physiological Responses to Snoezelen Multisensory StimulationLucia Ludvigh Cintulova,Jerzy Rottermund,Zuzana Budayova. Analysis of Psychological and Physiological Responses to Snoezelen Multisensory Stimulation. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001103; 8: 115-125
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."