Abstract
Review Article
Pulmonary Involvement in COVID-19 and ‘Long Covid’: The Morbidity, Complications and Sequelae
Vinod Nikhra*
Published: 15 June, 2021 | Volume 5 - Issue 1 | Pages: 034-048
Introduction: the perennial pandemic: There are serious challenges posed by the SARS-CoV-2 virus and COVID-19 as the disease. With the persistence of the pandemic over one and half year, it is being feared that the COVID-19 may have become the new reality associated with human existence world over and the mankind may have to live with it for years or even decades. Further, the grievous nature of the disease is evolving further with genomic changes in the virus in form of mutations and evolution of variants, with enhanced infectivity and probably virulence.
Acute and chronic phases of COVID-19: Epidemiologically, it is becoming clear that apart from the advanced age and pre-existing conditions, such as diabetes, cardiovascular, pulmonary, and renal diseases, certain constituent factors render some patients more vulnerable to more severe forms of the disease. These factors influence the COVID-19 manifestations, its course, and later the convalescence period as well as the newly defined ‘Long COVID phase. The substantial continuing morbidity after resolution of the infection indicates persisting multisystem effects of ‘Long Covid’.
Lung damage associated with COVID-19: COVID-19 is primarily a respiratory disease presenting with a broad spectrum of respiratory tract involvement ranging from mild upper airway affliction to progressive life-threatening viral pneumonia and respiratory failure. It affects the respiratory system in various ways across the spectrum of disease severity, depending on age, immune status, and comorbidities. The symptoms may be mild, such as cough, shortness of breath and fevers, to severe and critical disease, including respiratory failure, shock, cytokine crisis, and multi-organ failure.
Implications for the post-COVID care: Depending on the severity of respiratory inflammation and damage, as well as associated comorbidities, duration of injury and genetics, the progressive fibrosis leads to constriction and compression of lung tissues and damage to pulmonary microvasculature. Consequently, the COVID-19 patients with moderate/severe symptoms are likely to have a significant degree of long-term reduction in lung function. Depending on the severity of the disease, extensive and long-lasting damage to the lungs can occur, which may persist after resolution of the infection.
Managing the long COVID’s challenges: Given global scale of the pandemic, the healthcare needs for patients with sequelae of COVID-19, especially in those with lung affliction are bound to increase in the near future. The challenge can be tackled by harnessing the existing healthcare infrastructure, development of scalable healthcare models and integration across various disciplines with a combination of pharmacological and non-pharmacological modalities. Following clinical and investigational assessment, the therapeutic strategy should depend on the disease manifestations, extent of damage in lungs and other organs, and associated complications.
Read Full Article HTML DOI: 10.29328/journal.jprr.1001022 Cite this Article Read Full Article PDF
Keywords:
Long COVID; Long haulers; Ground glass opacities; COVID pneumonia; ARDS; Pulmonary fibrosis; COVID pulmonary clinics; Heart failure; Pulmonary care continuum; Holistic care
References
- Max Planck Institute for the Science of Human History. COVID-19 is here to stay for the foreseeable future: Future of field-based sciences in the time of coronavirus. Science Daily. 2020. www.sciencedaily.com/releases/2020/09/200914112206.htm
- Oran DP, Topol EJ. The Proportion of SARS-CoV-2 Infections That Are Asymptomatic. Ann Inter Med. 2021; 174: 655-662. PubMed: https://pubmed.ncbi.nlm.nih.gov/33481642/
- Pollitt KJG, Peccia J, Ko AI, Kaminski N, Dela Cruz CS, et al. COVID-19 vulnerability: the potential impact of genetic susceptibility and airborne transmission. Human Genom. 2020; 14: 17. PubMed: https://pubmed.ncbi.nlm.nih.gov/32398162/
- Wang C, Wang Z, Wang G, Lau JY, Zhang K, et al. COVID-19 in early 2021: current status and looking forward. Sig Transduct Target Ther. 2021; 6: 114. PubMed: https://pubmed.ncbi.nlm.nih.gov/33686059/
- Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020; 581: 465–469. PubMed: https://pubmed.ncbi.nlm.nih.gov/32235945/
- Gozalbo-Rovira R, Gimenez E, Latorre V, Francés-Gómez C, Albert E, et al. SARS-CoV-2 antibodies, serum inflammatory biomarkers and clinical severity of hospitalized COVID-19 patients. J Clin Virol. 2020; 131: 104611. PubMed: https://pubmed.ncbi.nlm.nih.gov/32882666/
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395: 507-513. PubMed: https://pubmed.ncbi.nlm.nih.gov/32007143/
- Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network — United States, March–June 2020. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. 2020; 69:
- Carfì A, Bernabei R, Landi F. for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020; 324: 603–605. PubMed: https://pubmed.ncbi.nlm.nih.gov/32644129/
- PubMed: https://www.uchealth.com/en/media-room/covid-19/short-and-long-term-lung-damage-from-covid-19
- Kommos FKF, Schwab C, Tavernar L, Schreck J, Wagner WL, et al. The Pathology of Severe COVID-19-Related Lung Damage. Dtsch Arztebl Int. 2020; 117: 500-506. PubMed: https://pubmed.ncbi.nlm.nih.gov/32865490/
- Aguiar D, Lobrinus JA, Schibler M, Fracasso T, Lardi C. Inside the lungs of COVID-19 disease. Int J Legal Med. 2020; 134: 1271-1274. PubMed: https://pubmed.ncbi.nlm.nih.gov/32458044/
- Guo J, Huang Z, Lin L, Lv J. Coronavirus Disease 2019 (COVID‐19) and Cardiovascular Disease: A Viewpoint on the Potential Influence of Angiotensin‐Converting Enzyme Inhibitors/Angiotensin Receptor Blockers on Onset and Severity of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. 9 Apr 2020. J Am Heart Assoc. 2000; 9: 9: e016219. PubMed: https://pubmed.ncbi.nlm.nih.gov/32233755/
- Jain U. Effect of COVID-19 on the Organs. Cureus. 2020; 12: e9540. PubMed: https://pubmed.ncbi.nlm.nih.gov/32905500/
- Frizzelli A, Tuttolomondo D, Aiello M, Majori M, Bertorelli G, et al. What happens to people's lungs when they get coronavirus disease 2019? Acta Biomed. 2020; 91: 146-149. PubMed: https://pubmed.ncbi.nlm.nih.gov/32420938/
- Sadhukhan P, Ugurlu MT, Hoque MO. Effect of COVID-19 on Lungs: Focusing on Prospective Malignant Phenotypes. Cancers (Basel). 2020; 12: 3822. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7766284/
- Huang C, Huang L, Wang Y, Li X, Ren L, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021; 397: P220-232. PubMed: https://pubmed.ncbi.nlm.nih.gov/33428867/
- Bussani R, Schneider E, Zentilin L, Collesi C, Ali H, et al. Persistence of viral RNA, pneumocyte syncytia and thrombosis are hallmarks of advanced COVID-19 pathology. Lancet – EbioMedicine. 2020; 61: 103104. PubMed: https://pubmed.ncbi.nlm.nih.gov/33158808/
- Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, et al. Pulmonary Vascular Endotheliitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020; 383: 120-128. PubMed: https://pubmed.ncbi.nlm.nih.gov/32437596/
- Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis. 2020; 20: 1135-1140. PubMed: https://pubmed.ncbi.nlm.nih.gov/32526193/
- Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19). 2021. PubMed: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
- Gattinoni L, Chiumello D, Rossi S. Editorial - COVID-19 pneumonia: ARDS or not? Critical Care. 2020; 24: 154. PubMed: https://pubmed.ncbi.nlm.nih.gov/32299472/
- Marini JJ, Gattinoni L. Management of COVID-19 Respiratory Distress. JAMA. 2020; 323: 2329-2330. PubMed: https://pubmed.ncbi.nlm.nih.gov/32329799/
- Cascella M, Rajnik M, Aleem A,.Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). 2021. PubMed: https://pubmed.ncbi.nlm.nih.gov/32150360/
- Torres Acosta MA, Singer BD. Pathogenesis of COVID-19-induced ARDS: implications for an aging population. Eur Respirat J. 2020; 56: 2002049. PubMed: https://pubmed.ncbi.nlm.nih.gov/32747391/
- Yang W, Sirajuddin A, Zhang X, Liu G, Teng Z, et al. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol. 2020; 30: 4874-4882. PubMed: https://pubmed.ncbi.nlm.nih.gov/32296940/
- Fu F, Lou J, Xi D, Bai Y, Ma G, et al. Chest computed tomography findings of coronavirus disease 2019 (COVID-19) pneumonia. Eur Radiol, 2020; 30: 5489-5498. PubMed: https://pubmed.ncbi.nlm.nih.gov/32435925/
- Kong W, Agarwal PP. Chest Imaging Appearance of COVID-19 Infection. Radiol Cardiothorac Imaging. 2020; 2: e200028. PubMed: https://pubmed.ncbi.nlm.nih.gov/33778544/
- de Pádua Gomes FL, Kaiser FE, Nunes U, Giunchetti Strabelli D, Loureiro BMC, et al. Imaging findings in COVID-19 pneumonia. Clinics. 2020; 75: e2027. PubMed: https://pubmed.ncbi.nlm.nih.gov/32578826/
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020; 215: 87-93. PubMed: https://pubmed.ncbi.nlm.nih.gov/32174129/
- Zhang P, Li J, Liu H, Han N, Ju J, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020; 8: 8. PubMed: https://pubmed.ncbi.nlm.nih.gov/32128276/
- Wells AU, Devaraj A, Desai SR. Interstitial Lung Disease after COVID-19 Infection: A Catalog of Uncertainties. Radiology. 2021; 299: E216–E218. PubMed: https://pubmed.ncbi.nlm.nih.gov/33502279/
- Truffaut L, Demey L, Bruyneel AV, Roman A, Alard S, et al. Post-discharge critical COVID-19 lung function related to severity of radiologic lung involvement at admission. Respir Res. 2021; 22: 29. PubMed: https://pubmed.ncbi.nlm.nih.gov/33478527/
- Pan F, Ye T, Sun P, Gui S, Liang B, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020; 295: 715-721. PubMed: https://pubmed.ncbi.nlm.nih.gov/32053470/
- Han X, Fan Y, Alwalid O, Li N, Jia X, et al. Six-month Follow-up Chest CT Findings after Severe COVID-19 Pneumonia. Radiology. 2021; 299: E177–E186. PubMed: https://pubmed.ncbi.nlm.nih.gov/33497317/
- Murray MF, Kenny EE, Ritchie MD, Rader DJ, Bale AE, et al. COVID-19 outcomes and the human genome. Genet Med. 2020; 22: 1175-1177. PubMed: https://pubmed.ncbi.nlm.nih.gov/32393819/
- Project Leader Dr Helen Su, National Institute of Allergy and Infectious Diseases (NIAID)/National Institutes of Health (NIH), Bethesda, USA and Co-leader Dr Jean-Laurent Casanova, The Rockefeller University, Howard Hughes Medical Institute (HHMI), New York, USA and Necker Hospital for Sick Children & INSERM, Paris, France. PubMed: https://www.covidhge.com
- Godlee F. Editors’s Choice - Living with COVID-19. BMJ. 2020; 370: m3392. PubMed: https://www.heighpubs.org/hjcv/abstract.php?id=ijcv-aid1030
- del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 2020; 324: 1723-1724. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031513/
- Gorna R, MacDermott N, Rayner C, O'Hara M, Evans S, et al. Comment: Long COVID guidelines need to reflect lived experience. The Lancet. 2021; 397: 455-457. PubMed: https://pubmed.ncbi.nlm.nih.gov/33357467/
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. medRxiv and bioRxiv. 2020.
- Cellai M, O’Keefe JB. Characterization of prolonged COVID-19 symptoms and patient comorbidities in an outpatient telemedicine cohort. medRxiv and bioRxiv. 2020.
- Carvalho-Schneider C, Laurent E, Lemaignenet A, Beaufils E, Bourbao-Tournois C, et al, Follow-up of adults with noncritical COVID-19 two months after symptom onset. Clin Microbiol Infect. 2021; 27: 258-263. PubMed: https://pubmed.ncbi.nlm.nih.gov/33031948/
- Wise J. Covid-19: Symptoms are common after acute phase of disease, Italian study shows. BMJ. 2020; 370: m2804. PubMed: https://pubmed.ncbi.nlm.nih.gov/32651164/
- Glöckl R, Buhr-Schinner H, Koczulla AR, Schipmann R, Schultz K, et al. [Recommendations from the German Respiratory Society for Pulmonary Rehabilitation in Patients with COVID-19]. Pneumologie. 2020; 74: 496-504. PubMed: https://pubmed.ncbi.nlm.nih.gov/32583378/
- Phelan D, Kim JH, Chung EH. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) infection. JAMA Cardiol. 2020; 5: 1085-1086. PubMed: https://pubmed.ncbi.nlm.nih.gov/32402054/
- Salman D, Vishnubala D, Le Feuvre P, Beaney T, Korgaonkar J, et al. Returning to physical activity after covid-19. BMJ. 2021; 372: m4721. PubMed: https://pubmed.ncbi.nlm.nih.gov/33419740/
- Tenforde MW, Kim SS, Lindsell CJ. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network — United States, Morb Mortal Wkly Rep. 2020; 69: 993-998.
- Williams N. The Borg Rating of Perceived Exertion (RPE) scale. Occup Med. 2017; 67: 404-405.
- Halpin, SJ, McIvor C, Whyatt G, Adams A, Harvey O, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021; 93: 1013-1022. PubMed: https://pubmed.ncbi.nlm.nih.gov/32729939/
- Lechowicz K, Drożdżal S, Machaj F, Rosik J, Szostak B, et al. COVID-19: The Potential Treatment of Pulmonary Fibrosis Associated with SARS-CoV-2 Infection. J Clin Med. 2020; 9: 1917. PubMed: https://pubmed.ncbi.nlm.nih.gov/32575380/
- Chen JY, Qiao K, Liu F, Wu B, Xu X, et al. Lung transplantation as therapeutic option in acute respiratory distress syndrome for COVID-19-related pulmonary fibrosis. Chin Med J. 2020; 133; 133: 1390-1396. PubMed: https://pubmed.ncbi.nlm.nih.gov/32251003/
- Bharat A, Machuca TN, Querrey M, Kurihara C, Garza-Castillon R Jr, et al. Early outcomes after lung transplantation for severe COVID-19: a series of the first consecutive cases from four countries. Lancet Respir Med. 2021; 9: 487-497. PubMed: https://pubmed.ncbi.nlm.nih.gov/33811829/
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, et al. Post-acute COVID-19 syndrome. Nat Med. 2021; 27: 601–615. PubMed: https://pubmed.ncbi.nlm.nih.gov/33753937/
Figures:
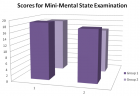
Figure 1

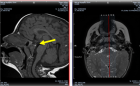
Figure 2

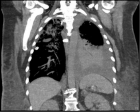
Figure 3

Figure 4

Figure 5

Figure 6
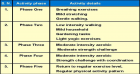
Figure 7

Figure 8
Similar Articles
-
Avoiding confusion in high flow oxygen therapy conceptsGarcía G,Valencia P,Mercedes E, Sarhane Y,Díaz-Lobato S*,Agosta M. Avoiding confusion in high flow oxygen therapy concepts. . 2017 doi: 10.29328/journal.jprr.1001001; 1: 001-002
-
Pulmonary Involvement in COVID-19 and ‘Long Covid’: The Morbidity, Complications and SequelaeVinod Nikhra*. Pulmonary Involvement in COVID-19 and ‘Long Covid’: The Morbidity, Complications and Sequelae. . 2021 doi: 10.29328/journal.jprr.1001022; 5: 034-048
-
SARS-CoV-2 Infection, COVID-19, and long covid: Saga of erratic immune response, waning immunity, and immune system failureVinod Nikhra*. SARS-CoV-2 Infection, COVID-19, and long covid: Saga of erratic immune response, waning immunity, and immune system failure. . 2021 doi: 10.29328/journal.jprr.1001030; 5: 078-087
-
Chronic thromboembolic pulmonary hypertension resulting in decompensated right heart failureDaniel Miller,Karim Makhoul,Allison Foster,Asma Ul Hosna*. Chronic thromboembolic pulmonary hypertension resulting in decompensated right heart failure. . 2022 doi: 10.29328/journal.jprr.1001037; 6: 012-015
-
Role of Inflammatory Markers in Predicting Severity in COVID-19 Patients at Tertiary Care Hospital, Ujjain (M.P.)Shivmohan Sarraf*, Mustafa Singapurwala, Harshit Jain, Ravendra Singh, Arti Julka. Role of Inflammatory Markers in Predicting Severity in COVID-19 Patients at Tertiary Care Hospital, Ujjain (M.P.). . 2023 doi: 10.29328/journal.jprr.1001043; 7: 004-009
Recently Viewed
-
Correlation of Inappropriate use of Ceftriaxone and Bacterial Resistance in the Hospital Environment: Integrative ReviewLarissa Furtado Abrantes, Joyce Lima de Sousa, Joel Messias Soares Ramos, Rafael Rodrigues Leite, Sávio Benvindo Ferreira*. Correlation of Inappropriate use of Ceftriaxone and Bacterial Resistance in the Hospital Environment: Integrative Review. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001051; 8: 014-020
-
The Cortisol Connection: Weight Gain and Stress HormonesBalvinder Singh, Neelesh Kumar Maurya*. The Cortisol Connection: Weight Gain and Stress Hormones. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001050; 8: 009-013
-
Evaluation of the Anti-inflammatory Activity of Equisetum arvense and Baccharis trimera FractionsCarolina Ferreira Vaz, Alan Fernandes Mariano, Júlia Amanda Rodrigues Fracasso, Marcus Vinicius Vieitas Ramos, Lucineia dos Santos, Herbert Júnior Dias*. Evaluation of the Anti-inflammatory Activity of Equisetum arvense and Baccharis trimera Fractions. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001049; 8: 003-008
-
Acyclovir Induced Acute Kidney Injury: A Case ReportZiauddin Mohammed*, Mariya Zoha Muskan, Megha Mohan Narayanan. Acyclovir Induced Acute Kidney Injury: A Case Report. Arch Pharm Pharma Sci. 2024: doi: 10.29328/journal.apps.1001048; 8: 001-002
-
Molecular Mechanisms and Potential Predictive Biomarkers in Advanced Non-small Cell Lung Cancer: A Summary of Current and Future TrendsIsabella Sforzin*, Juliana Rodrigues Beal, Fernando Moura. Molecular Mechanisms and Potential Predictive Biomarkers in Advanced Non-small Cell Lung Cancer: A Summary of Current and Future Trends. Arch Surg Clin Res. 2024: doi: 10.29328/journal.ascr.1001082; 8: 039-061
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."