More Information
Submitted: June 13, 2022 | Approved: July 01, 2022 | Published: July 04, 2022
How to cite this article: Gomes RR. Tuberculosis: A rarest cause of pulmonary vocal syndrome. J Pulmonol Respir Res. 2022; 6: 004-006.
DOI: 10.29328/journal.jprr.1001035
Copyright License: © 2022 Gomes RR. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Vocal cord paralysis; Dysphonia; Recurrent laryngeal nerve; Mediastinal lymphadenopathy
Tuberculosis: A rarest cause of pulmonary vocal syndrome
Richmond R Gomes*
Associate Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
*Address for Correspondence: Richmond Ronald Gomes, Dr. Associate Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh, Email: [email protected]
Hoarseness of voice can occur due to anatomical or functional abnormality of the larynx, vocal cord, or recurrent laryngeal nerves. Common cause includes infections, blunt trauma, iatrogenic affection of recurrent laryngeal nerve, malignancies of thyroid, esophagus, and lung and cardio-vascular conditions such as mitral stenosis. Vocal cord paralysis due to respiratory cause is known as a pulmonary vocal syndrome.
Tuberculosis is a disease often involving various organs, presenting with a wide variety of clinical manifestations. The intrathoracic disease usually affects only the left recurrent laryngeal nerve because of its long intrathoracic course as it hooks around the aorta. The right recurrent laryngeal nerve hooks around the subclavian artery and may be affected in apical pleural fibrosis or by supraclavicular lymph nodes (when left and right nerves are affected with equal frequency) or rarely mediastinal lymph nodes [1-3]. As the prevalence of pulmonary tuberculosis has declined over the past few years, more extra pulmonary cases are being reported. Tuberculous lymphadenopathy is the most common form of extra pulmonary tuberculosis, of which hilar and mediastinal lymph nodes are more commonly affected [4].
Identifying the varying presentations of tuberculosis can help us identify the disease early and initiate appropriate treatment. We present a case of pulmonary vocal syndrome due to pulmonary tuberculosis and thus aims to identify varying presentation of pulmonary tuberculosis and the reversibility of these lesions with antituberculous treatment.
A 50-year-old service holder, not known to have diabetes mellitus, hypertension, bronchial asthma, or coronary artery disease presented with symptoms of three months duration of cough and hoarseness of voice. He is a smoker for the last 20 years and smokes around 20 sticks per day. There was no history of fever, weight loss, anorexia, malaise, hemoptysis, preceding viral illness, vocal cord abuse, paroxysmal nocturnal dyspnoea, or rheumatic heart disease. He also denied any previous history of tuberculosis or contact with a patient with active tuberculosis. BCG vaccination status of the patient was not known. On general examination, he had no pallor or clubbing. No cervical lymphadenopathy was found. A respiratory system examination revealed bronchial breathing over the right upper chest from the front with increased vocal resonance. Other systemic examinations revealed no abnormalities.
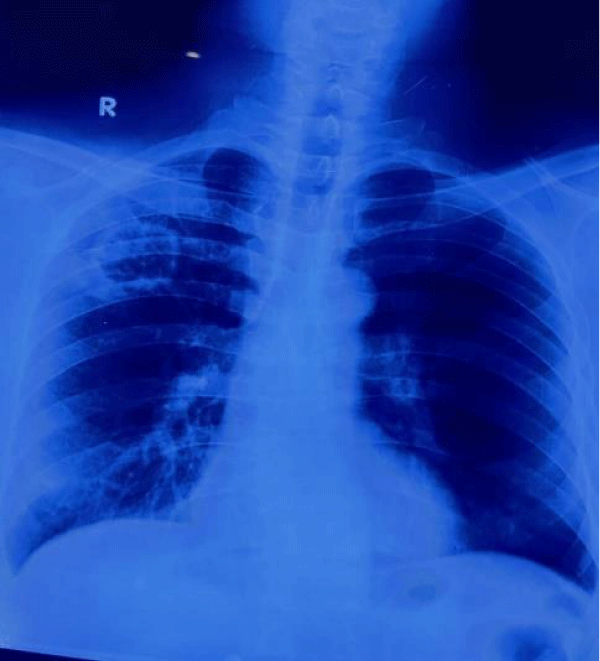
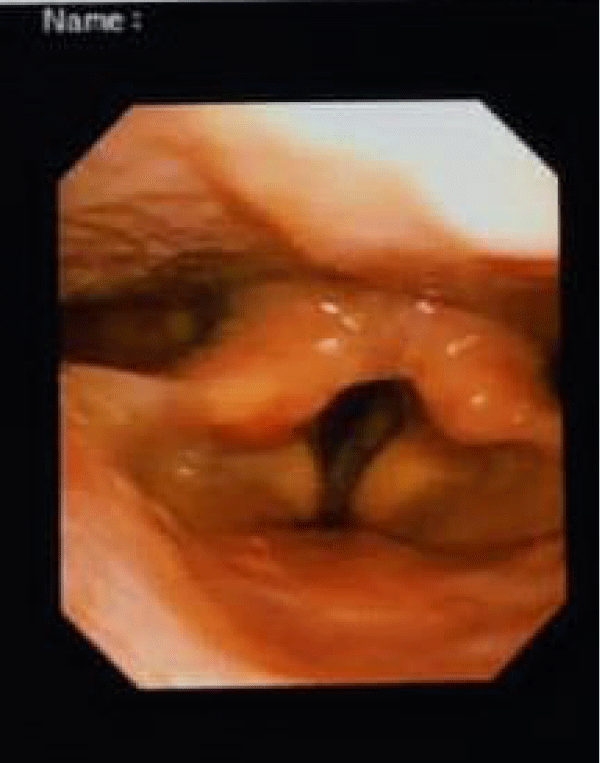
On laboratory investigations, complete blood count was normal except ESR 75 mm in 1st hour. Liver function tests, renal function tests, and random blood sugar were normal. Sputum culture failed to reveal the growth of any microorganism. Chest X-ray revealed an irregular walled cavitary lesion in part of the right upper and right mid zone (Figure 1, black arrow). Fiber optic laryngoscopy revealed thickened left vocal cord with restricted movement suggestive of left vocal cord palsy (Figure 2).
Figure 1: Chest x-ray showing irregular walled cavitary lesion over the right upper and mid zone.
Figure 2: Fiber optic laryngoscopy revealed thickened left vocal cord with restricted movement suggestive of left vocal cord palsy.
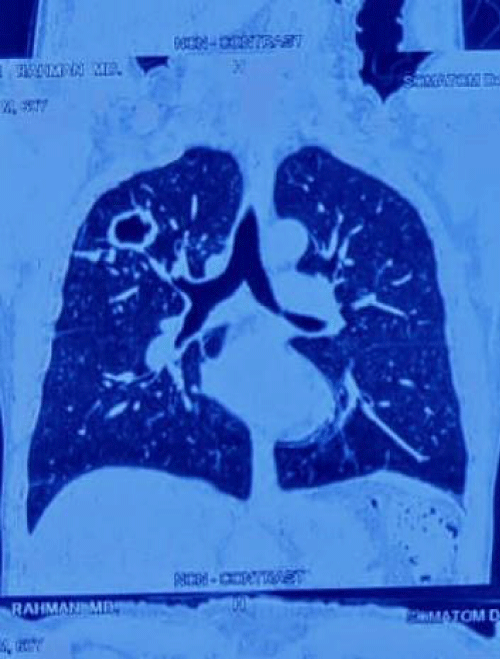
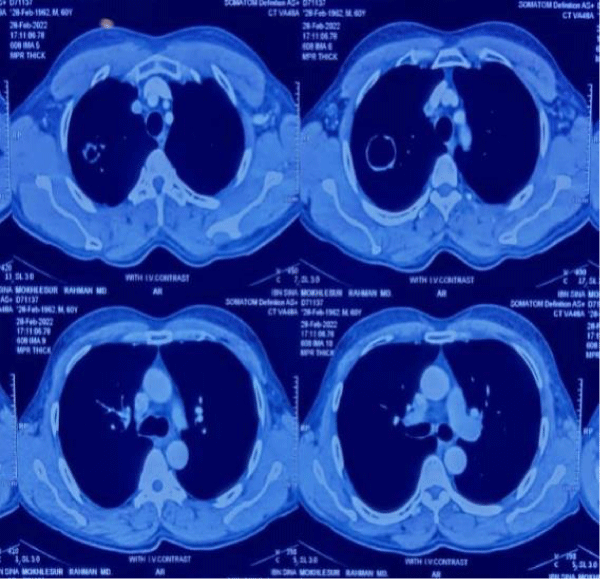
Tuberculin test demonstrated an induration of 10×12 mm. Sputum examination was likewise negative for acid-fast bacilli but gene Xpert became positive. CT chest revealed a thick ragged walled cavitary lesion in the right upper lung with associated regional inflammation (Figure 3, black arrow) and narrowed left major bronchus. Mediastinal lymphadenopathy was present (Figure 4, black arrow).
Figure 3: Chest chest showing right-sided cavitary lesion with narrowing of left major bronchus and mediastinal lymphadenopathy respectively.
Figure 4: Chest chest showing right-sided cavitary lesion with narrowing of left major bronchus and mediastinal lymphadenopathy respectively.
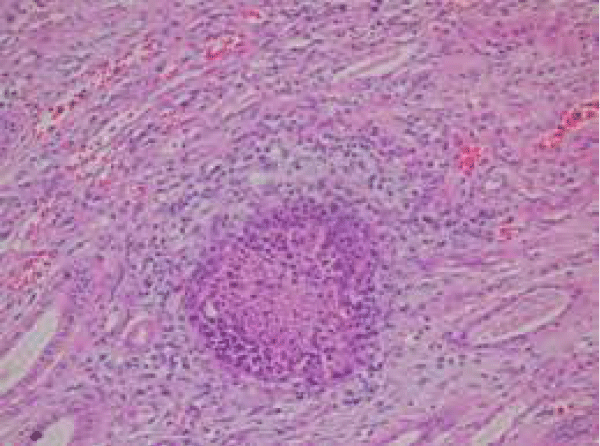
FNAC from a right-sided cavitary lesion of the lung revealed caseating granuloma suggestive of tuberculosis (Figure 5, black arrow).
Figure 5: istopathology of right lung cavitary lesion revealing caseating granuloma.
The diagnosis of left vocal cord palsy due to right-sided pulmonary tuberculosis with mediastinal lymphadenopathy was made and anti tuberculous drug therapy was initiated according to weight following national guideline protocol. After 6 months of therapy, vocal cord function had partially recovered.
Hoarseness of voice is a frequently encountered symptom seen due to structural or functional involvement of the larynx, vocal cord, or secondary to involvement of recurrent laryngeal nerve. Common causes include iatrogenic such as following thyroid surgeries (41%), idiopathic causes (33%), and well-defined causes (25%) [5] such as lung malignancy, thyroid malignancy, oesophageal malignancy, cardiac causes such as Ortners syndrome and chronic benign inflammatory conditions such as tuberculosis. Earlier hoarseness of voice after ruling out malignancy of the lung was largely attributed to cardiovascular causes such as mitral stenosis, left atrial enlargement, or pulmonary hypertension. This entity was known as Ortner’s syndrome. Hoarseness of voice due to the involvement of recurrent laryngeal nerve secondary to a respiratory cause is known as a pulmonary vocal syndrome.
The involvement of the left recurrent laryngeal nerve is more common when compared to the right as it arches around the arch of the aorta and has a substantial intrathoracic course [6]. Such an entity is more often encountered in association with bronchogenic carcinoma [7]. However, it can also be seen in association with chronic benign inflammatory conditions such as tuberculosis. Later Radner [8] quoted in his article about the possibility of tuberculosis leading to recurrent laryngeal nerve palsy. The right recurrent laryngeal nerve could be involved in right upper lobe fibrosis or rarely due to right mediastinal adenopathy [9,10].
The various mechanisms responsible for tuberculosis that might lead to the pulmonary vocal syndrome are [11-13].
1. The nerve passes through the caseating lymph node.
2. The nerve might get stretched due to dense pleural thickening or fibrosing mediastinitis.
3. The nerve is stretched due to retraction of the upper lobe bronchus towards the apex as in endobronchial tuberculosis.
4. The nerve is compressed by an enlarged pulmonary artery.
The aortopulmonary window is a small space between the aortic arch and the pulmonary artery. A variety of structures traverse this window including the left recurrent laryngeal nerve. Enlargement of lymph nodes secondary to our patients’ tuberculosis infection may compress the recurrent laryngeal nerve causing vocal cord paralysis, resulting in hoarseness.
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS- TBNA)using a dedicated bronchoscope with a convex ultrasound probe at its tip allows real-time sampling from enlarged mediastinal nodes under direct visualization. It has high sensitivity and specificity in the diagnosis of mediastinal lymphadenopathy due to tuberculosis [4]. The aspirates can be subjected to detailed cytological and microbiological examinations. EBUS –TBNA was not available in our center.
Recurrent laryngeal nerve(RLN) paralysis due to mediastinal lymph node tuberculosis is reversible and has been reported to respond favorably to anti-TB treatment in most cases. Our patient had an uneventful recovery and vocal cord function normalized on follow-up. This highlights the importance of keeping tuberculosis as a differential diagnosis in the evaluation of hoarseness, especially in [2] developing countries. A chest radiograph alone is insufficientfor clinical evaluation in these circumstances. Even in resource-limited settings, patients with vocal cord palsy should be referred to a facility where essential investigations can be performed and the underlying cause can be ascertained. Tubercular mediastinal lymphadenopathy is an important, reversible cause of isolated left vocal cord palsy.
The recurrent laryngeal nerve is commonly involved in thoracic tuberculosis in both parenchymal and mediastinal nodes. In the investigation of the causes of recurrent laryngeal nerve paralysis, pulmonary tuberculosis must be a conside-ration, especially in a patient presenting with hoarseness as a differential diagnosis. Thus, clinicians must always consider the possibility of impingement or compression of the recurrent laryngeal nerve from tuberculous lymphadenopathy.
- Song SW, Jun BC, Cho KJ, Lee S, Kim YJ, Park SH. CT evaluation of vocal cord paralysis due to thoracic diseases: a 10-year retrospective study. Yonsei Med J. 2011 Sep;52(5):831-7. doi: 10.3349/ymj.2011.52.5.831. PMID: 21786449; PMCID: PMC3159943.
- Rafay MA. Tuberculous lymphadenopathy of superior mediastinum causing vocal cord paralysis. Ann Thorac Surg. 2000 Dec;70(6):2142-3. doi: 10.1016/s0003-4975(00)01193-0. PMID: 11156137.
- Fowler RW, Hetzel MR. Tuberculous mediastinal lymphadenopathy can cause left vocal cord paralysis. Br Med J (Clin Res Ed). 1983 May 14;286(6377):1562. doi: 10.1136/bmj.286.6377.1562. PMID: 6405888; PMCID: PMC1547986.
- Navani N, Molyneaux PL, Breen RA, Connell DW, Jepson A, Nankivell M, Brown JM, Morris-Jones S, Ng B, Wickremasinghe M, Lalvani A, Rintoul RC, Santis G, Kon OM, Janes SM. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: a multicentre study. Thorax. 2011 Oct;66(10):889-93. doi: 10.1136/thoraxjnl-2011-200063. Epub 2011 Aug 3. PMID: 21813622; PMCID: PMC3361304.
- Havas T, Lowinger D, Priestley J. Unilateral vocal fold paralysis: causes, options and outcomes. Aust N Z J Surg. 1999 Jul;69(7):509-13. doi: 10.1046/j.1440-1622.1999.01613.x. PMID: 10442923.
- Brunicardi FC, Brunicardi F, Andersen D, et al. Schwartz's Principles of Surgery (9th ed.). McGraw Hill Professional. September 11, 2009; ISBN 978-0-07-154769-7.
- Spiro SG, Gould MK, Colice GL; American College of Chest Physicians. Initial evaluation of the patient with lung cancer: symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007 Sep;132(3 Suppl):149S-160S. doi: 10.1378/chest.07-1358. PMID: 17873166.
- RADNER DB, SNIDER GL. Recurrent laryngeal nerve paralysis as a complication of pulmonary tuberculosis; a report of two cases. Am Rev Tuberc. 1952 Jan;65(1:1):93-9. doi: 10.1164/art.1952.65.1.93. PMID: 14885712.
- Shin JE, Nam SY, Yoo SJ, Kim SY. Changing trends in clinical manifestations of laryngeal tuberculosis. Laryngoscope. 2000 Nov;110(11):1950-3. doi: 10.1097/00005537-200011000-00034. PMID: 11081616.
- Hajjar WM, AlShalan HA, Alsowayyan MA, Al-Nassar SA. Unusual cause of bilateral vocal cord paralysis. Saudi J Anaesth. 2016 Oct-Dec;10(4):459-461. doi: 10.4103/1658-354X.177323. PMID: 27833496; PMCID: PMC5044737.
- Joshi JM, Doshi AV, Kamble RT. Spontaneous vocal cord paralysis in pulmonary tuberculosis: The Pulmonary vocal syndrome. JAPI 1997; 8:625-28.
- GUPTA SK. The syndrome of spontaneous laryngeal palsy in pulmonary tuberculosis. J Laryngol Otol. 1960 Feb;74:106-13. doi: 10.1017/s0022215100056309. PMID: 13830330.
- Farmer WC, Fulkerson LL, Stein E. Vocal cord paralysis due to pulmonary tuberculosis. Am Rev Respir Dis. 1975 Oct;112(4):565-9. doi: 10.1164/arrd.1975.112.4.565. PMID: 1200488.