More Information
Submitted: October 14, 2024 | Approved: October 21, 2024 | Published: October 22, 2024
How to cite this article: Haripriya Menon V, Unnikrishnan R. Occult Pneumomediastinum - An Atypical Presentation of Chest Discomfort in a Patient with Depression. J Pulmonol Respir Res. 2024; 8(2): 060-062. Available from: https://dx.doi.org/10.29328/journal.jprr.1001062
DOI: 10.29328/journal.jprr.1001062
Copyright License: © 2024 Haripriya Menon V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pneumomediastinum; Mediastinal emphysema; Shortness of breath; Chest discomfort
Occult Pneumomediastinum - An Atypical Presentation of Chest Discomfort in a Patient with Depression
Haripriya Menon V* and Unnikrishnan R
Junior Resident, Department of Respiratory Medicine, Government Medical College, Kota, Rajasthan, India
*Address for Correspondence: Dr. Haripriya Menon V, Junior Resident, Department of Respiratory Medicine, Government Medical College, Kota, Rajasthan, India, Email: [email protected]
Pneumomediastinum (mediastinal emphysema) is an uncommon condition characterized by the accumulation of air or gas in the mediastinum. Here is a case of a 16-year-old female known to have depression who presented to the emergency department with complaints of shortness of breath, restlessness, chest discomfort, and hoarseness of voice for 2 days. She was initially diagnosed with panic attack, and later on clinical examination, surgical emphysema over the right supraclavicular area was noticed. Chest X-ray was found to be normal, and further imaging with high-resolution computed tomography (HRCT) of the thorax showed pneumomediastinum. In this report, the clinical presentations, radiological features, and management of pneumomediastinum will be discussed.
Pneumomediastinum (mediastinal emphysema) refers to the presence of air in the mediastinum. The mediastinum is the space in the central thorax bounded laterally by the parietal pleura of the lungs, superiorly by the thoracic outlet, inferiorly by the diaphragm, anteriorly by the sternum, and posteriorly by the thoracic vertebral column [1]. Spontaneous or primary pneumomediastinum occurs in otherwise healthy individuals with no identifiable cause. Secondary pneumomediastinum includes all cases in which an underlying cause such as trauma can be elicited. The most common cause of pneumomediastinum is alveolar rupture. The incidence of spontaneous pneumomediastinum is 22 cases per 1,000,000 emergency visits.
Sometimes pneumomediastinum can present together with psychiatric disorders and often remain undiagnosed.
A 16-year-old female presented to the hospital with shortness of breath, restlessness, chest discomfort, and hoarseness of voice for 2 days. It was associated with retrosternal chest pain, radiating to the right supraclavicular region, a cracking sensation over the neck, and nonproductive coughing. The pain was exacerbated by deep inspiration and eased by sitting forward. The patient initially denied any precipitating event or comorbidities but later gave a history of depression, which was diagnosed 3 months later but not on regular medication. On examination, the patient was pale, distressed, and tachypneic (respiratory rate 24/min). The pulse rate was 110, saturation was 96% on room air, and the blood pressure was 110/70.
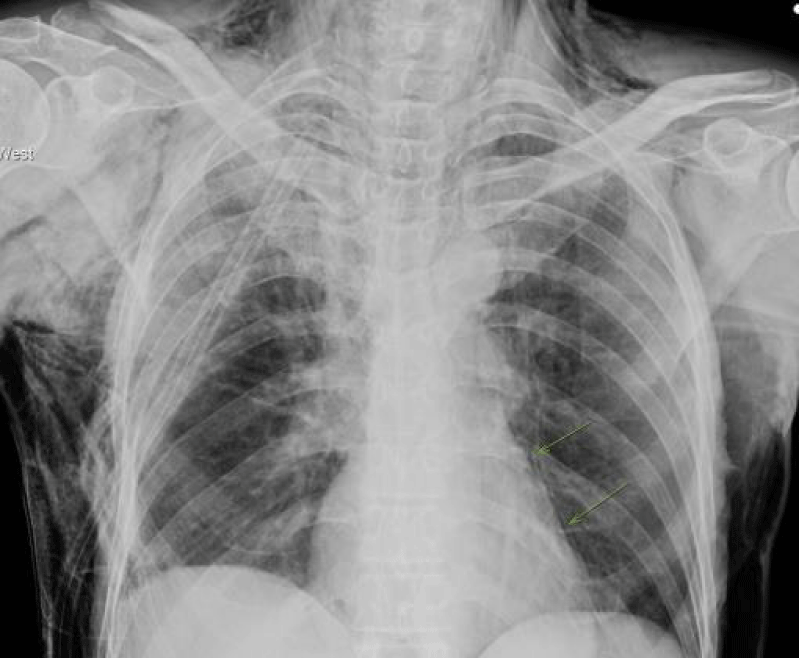
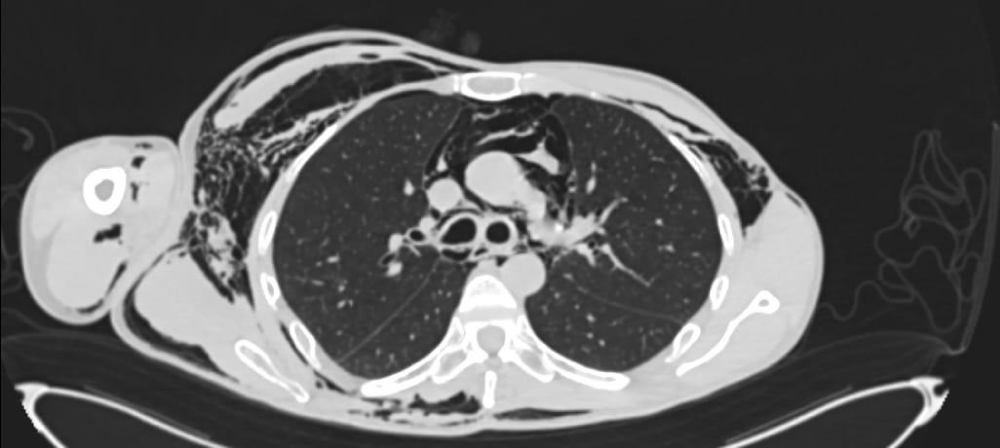
Surgical emphysema was faintly palpable in the right supraclavicular fossa. Air entry was reduced symmetrically, and there were scattered wheezes throughout both lung fields. A chest X-ray was taken and found to be normal. An electrocardiogram indicated normal sinus tachycardia. Chest HRCT was performed on an emergency basis and revealed pneumomediastinum with air collection in the neck region and posterior chest wall emphysematous changes (Images 1 and 2).
Image 1: Chest Xray of the patient showing pneumomediastinum.
Image 2: CT scan of the patient showing pneumomediastinum
She was admitted to the respiratory medicine ward, where she received oxygen by face mask for the next 4 days, following which the patient was symptomatically better with complete reduction of surgical emphysema in the right supraclavicular fossa.
Repeat HRCT was performed, which showed complete resolution of pneumomediastinum. Her SpO2 remained normal (97%) in room air, and she was discharged and referred to psychiatry. The patient was reviewed a week later when she remained asymptomatic and no abnormalities were present on examination. Both chest and neck radiographs were normal.
Pneumomediastinum is frequently associated with other forms of extra-alveolar air, including pulmonary interstitial emphysema, pneumopericardium, pneumothorax, subcutaneous emphysema, pneumoretroperitoneum, and pneumoperitoneum [2]. The majority of patients with pneumomediastinum have predisposing factors that cause an increase in airway pressure, which leads to alveolar rupture. Most commonly, this results from straining against a closed glottis (i.e., the Valsalva maneuver) during vomiting, coughing, or exercising [3]. Other mechanisms include sudden and/or severe increases in lung volume, as occur during marijuana smoking, vaping, inhaling of cocaine, anxiety attacks, seizures, active labor, chest trauma, and surgeries.
If pneumomediastinum is visible on chest X-ray, it is termed overt pneumomediastinum, whereas if it is only visible on CT, then it is termed occult pneumomediastinum [4]. On the posterior-anterior view of the chest X-ray, the most common findings are the following: air streaks in the superior mediastinum (sometimes they reach the neck), a prominent silhouette of the heart (especially on the left), continuous diaphragm sign, Naclerio V sign and subcutaneous emphysema of the shoulder and neck. Computed tomography (CT) is more sensitive in detecting air than plain radiographs and can provide information on alternative diagnoses. Air may be evident deep in the neck as well as in the subcutaneous tissue [5].
In this case, the patient had a known case of depression on irregular treatment. Although it is uncommon, pneumomediastinum can occur in patients with depression and anxiety disorders, the etiology of which is unknown [6]. When associated with psychiatric disorders.
Patients can have atypical presentations, and diagnoses can be missed.
Treatment of spontaneous pneumomediastinum is supportive and is primarily directed at pain relief and reassurance. Appropriate management of contributing causes such as foreign bodies, asthma, and parenchymal lung disorders should be instituted [7]. Needle aspiration, skin incision, or tube thoracotomy is almost never necessary and is discouraged until there is a concomitant pneumothorax [8].
Spontaneous pneumomediastinum follows a benign clinical course in most cases. This case highlights the complex interplay between physical and mental health in a 16-year-old female presenting with symptoms of pneumomediastinum and surgical emphysema. The absence of clear physical precipitating factors, combined with her history of depression, suggests that psychological stress may have played a significant role in her condition. Successful management involved supportive care and oxygen therapy, leading to the complete resolution of symptoms and pneumomediastinum. The patient’s follow-up demonstrated sustained improvement, underscoring the importance of integrating psychiatric evaluation and treatment in similar cases. This case serves as a reminder of the necessity for a comprehensive approach in adolescent patients with respiratory symptoms, recognizing the impact of mental health on physical well-being. When pneumomediastinum is associated with psychiatric disorders, diagnosis can be missed due to atypical presentations and prepossession. Therefore, a thorough clinical examination and proper radiological evaluation are needed in these scenarios.
Ethical consideration: Informed consent was obtained from the patient.
- Kouritas VK, Papagiannopoulos K, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, et al. Pneumomediastinum. J Thorac Dis. 2015;7(Suppl 1). Available from: https://doi.org/10.3978/j.issn.2072-1439.2015.01.11
- Okafor C, Soin S, Ferraz JFFM. Spontaneous pneumomediastinum complicating asthma exacerbation. BMJ Case Rep. 2019;12(2). Available from: https://doi.org/10.1136/bcr-2018-229118
- Iteen AJ, Bianchi W, Sharman T. Pneumomediastinum. 2023 May 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 32491372. Available from: http://www.ncbi.nlm.nih.gov/books/nbk557440/
- Gorrochategui M, Weerakkody Y, Chieng R, et al. Pneumomediastinum. Reference article, Radiopaedia.org [Accessed on 28 Sep 2023].
- Subhawong TK, Fishman EK, Swart JE, Carrino JA, Attar S, Fayad LM. Soft-tissue masses and masslike conditions: what does CT add to diagnosis and management? AJR Am J Roentgenol. 2010;194(6):1559-1567. Available from: https://doi.org/10.2214/ajr.09.3736
- Berliner D, Schneider N, Welte T, Bauersachs J. The differential diagnosis of dyspnea. Dtsch Arztebl Int. 2016 Dec 9;113(49):834-845. Available from: https://doi.org/10.3238/arztebl.2016.0834
- Sahni S, Verma S, Grullon J, Esquire A, Patel P, Talwar A. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci. 2013;5(8):460-464. Available from: https://doi.org/10.4103/1947-2714.117296
- Zehtabchi S, Rios CL. Management of emergency department patients with primary spontaneous pneumothorax: needle aspiration or tube thoracostomy? Ann Emerg Med. 2008 Jan;51(1):91-100, 100.e1. Available from: https://doi.org/10.1016/j.annemergmed.2007.06.009