More Information
Submitted: December 23, 2024 | Approved: February 04, 2025 | Published: February 05, 2025
How to cite this article: Kumar S, Alwa KS, Vemuri MB, Gupta AGG, Vallapudasu N, Geddada S. Unveiling the Impostor: Pulmonary Embolism Presenting as Pneumonia: A Case Report and Literature Review. J Pulmonol Respir Res. 2025; 9(1): 001-005. Available from:
https://dx.doi.org/10.29328/journal.jprr.1001065
DOI: 10.29328/journal.jprr.1001065
Copyright License: © 2025 Kumar S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pulmonary embolism (PE); Severe pneumonia; Lower respiratory tract infection; Differential diagnosis
Unveiling the Impostor: Pulmonary Embolism Presenting as Pneumonia: A Case Report and Literature Review
Saahil Kumar1, Karuna Sree Alwa2*, Mahesh Babu Vemuri3, Anumola Gandhi Ganesh Gupta2, Nuthan Vallapudasu2 and Sunitha Geddada1
1Junior Resident, Pulmonary Medicine, AIIMS, Bibinagar, India
2Senior Resident, Pulmonary Medicine, AIIMS, Bibinagar, India
3Assistant Professor, Pulmonary Medicine, AIIMS, Bibinagar, India
*Address for Correspondence: Karuna Sree Alwa, Senior Resident, Pulmonary Medicine, AIIMS, Bibinagar, India, Email: [email protected]
Pulmonary Embolism (PE) can present with symptoms resembling pneumonia, creating a diagnostic challenge, particularly in patients with comorbidities. We report the case of a 67-year-old male who presented with cough, hemoptysis, shortness of breath, fever, and pedal edema. Initially diagnosed with consolidation based on chest X-ray findings, he was treated with antibiotics. However, persistent symptoms prompted further evaluation, leading to the diagnosis of PE with pulmonary infarction and deep vein thrombosis on computed tomography pulmonary angiography and Doppler ultrasound. This case highlights the need to consider PE in the differential diagnosis of consolidation, particularly in high-risk individuals, to avoid delays in appropriate management.
Pulmonary embolism is a potentially life-threatening condition that often presents with nonspecific symptoms, complicating its diagnosis. This diagnosis becomes more challenging when it mimics other lung conditions, such as a lower respiratory tract infection. Here, we report a case of pulmonary embolism initially misdiagnosed as a lower respiratory tract infection, as advocated by the consolidation seen on chest X-ray, emphasising the need to consider pulmonary embolism in the differential diagnosis of pneumonia. Along with this case report, we review the literature available to explore the diverse clinical presentations and diagnostic complexities associated with pulmonary embolism falsely treated as pneumonia.
A 67-year-old male presented to our outpatient department with complaints of cough with haemoptysis, fever persisting for five days, associated with shortness of breath grade 2 MMRC. He also reported wheezing and bilateral pitting pedal oedema that had persisted for two weeks. There was no associated history of chest pain or palpitations.
The patient had previously sought care at a local polyclinic, where a chest X-ray showed a non-homogeneous opacity in the right lower lung zone. This led to a provisional diagnosis of community-acquired pneumonia. He was admitted and started on intravenous antibiotics, and subsequently discharged with a referral to our hospital for further evaluation and management as the patient was not improving.
Past medical history
The patient had a significant medical history, including:
- Type 2 Diabetes Mellitus prescribed OHA’s
- Hypertension prescribed antihypertensives
- Coronary artery disease: Status post-percutaneous transluminal coronary angioplasty 10 years ago.
Despite being prescribed regular medications for his chronic health issues, he was not compliant with any of the above treatments.
He also had a significant smoking history of 20 pack years, and he is a retired civilian with a sedentary lifestyle.
Examination findings
On examination, the patient appeared tachypnoeic, with signs of respiratory distress. His vital signs were unremarkable, except for a mildly elevated respiratory rate. Physical examination revealed:
Respiratory system: Bilateral polyphonic wheeze with reduced breath sounds and coarse crackles over the right infra-scapular area.
- Cardiovascular system: No murmurs or other abnormalities.
- Abdomen: Mild distension without tenderness or palpable organomegaly
- Peripheral oedema: Bilateral pitting pedal oedema up to mid-thigh.
Initial investigations
Routine blood tests and investigations were conducted to evaluate the underlying cause of the patient’s symptoms:
- Complete blood count: Within normal limits, significant leucocytosis.
- Renal and liver function tests: Unremarkable.
- Blood sugar levels: Elevated, consistent with uncontrolled diabetes.
- Electrocardiogram: Showed T wave inversion and Q wave in Lead III.
- Radiological assessment: The chest X-ray obtained at the polyclinic showed a non-homogeneous opacity in the right lower zone AS SHOWN, which coincides with clinical findings of coarse crackles in that area consistent with the earlier diagnosis of pneumonia.
The initial impression was severe community-acquired pneumonia given the tachypnoea associated with fever and leucocytosis. Intravenous Ceftriaxone 2 gm once daily was started. Routine blood and sputum cultures were done.
The patient did not improve symptomatically after admission and cultures turned out to grow normal flora after 48 hours of incubation. Based on the signs and symptoms and a Wells score of 4, ECG showing Q WAVE in lead III, a provisional diagnosis of Pulmonary Embolism was established and the patient was advised computed tomography pulmonary angiography, and the patient was admitted to the HDU under our care.
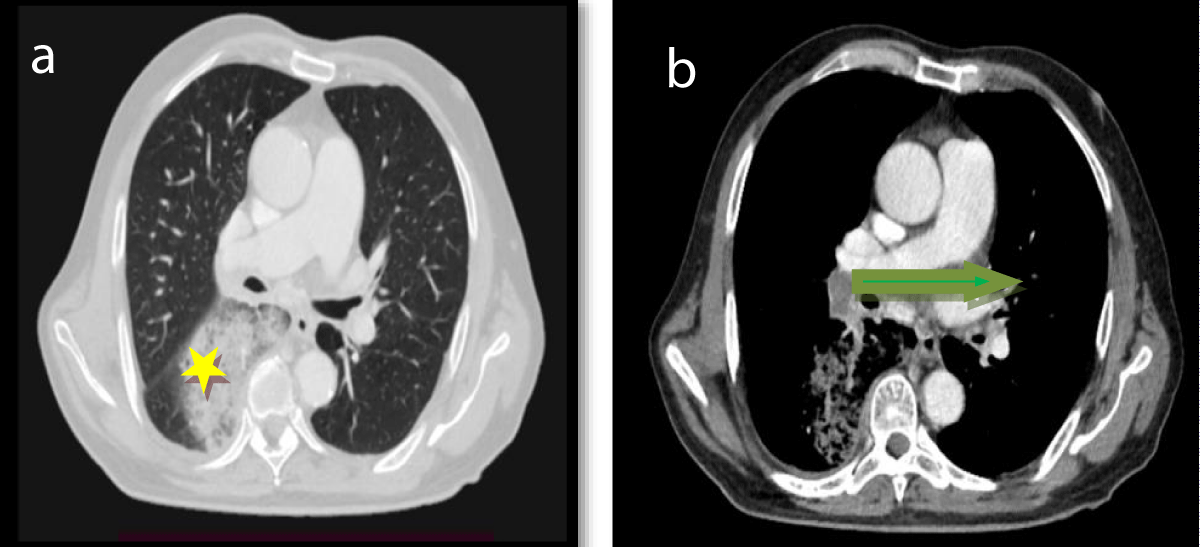
2D echocardiography was suggestive of Global Hypokinesia, Grade 3 Diastolic dysfunction, moderate AR, moderate PAH, moderate MR/TR/PR, Severe LV Systolic dysfunction, and an Ejection fraction of 30 %. CTPA revealed Non enhancing, hyperdense filling defect in the right main pulmonary trunk, seen extending into the right lower lobe segmental and sub-segmental arteries (Figures 1a,b).
Figure 1: CECT Contrast-enhanced CT Pulmonary Angiography (CTPA) – Axial section [a] [b]. A filling defect is noted in the right pulmonary artery extending into its segmental branches. The main pulmonary artery appears slightly dilated, distal to the affected pulmonary artery, patchy consolidation and ground-glass opacities are observed in the right lower lobe, suggesting pulmonary infarction due to compromised blood flow ⭐. Represents pulmonary infarction, and → representing filling defect.
To look for DVT a Doppler Venous Ultrasound of the Left lower Limb was requested and it revealed the following: Dilated short saphenous vein, diffuse wall thickening, partial echogenic content, partially compressible and thrombosed, a dilated tortuous vein in the posterior medial aspect of left lower limb (draining into Short Saphenous vein) showing thrombosis.
He was immediately initiated on subcutaneous Enoxaparin 60 mg on a twice-daily basis and then was shifted to Apixaban 5mg orally. The oral apixaban was continued for 3 months. His existing conditions, including diabetes, hypertension, and coronary artery disease, were optimized with appropriate medical therapy and lifestyle modifications. The patient has shown great recovery.
Differential diagnosis
The clinical presentation of Pulmonary Embolism (PE) often overlaps with other common pulmonary conditions, making accurate diagnosis challenging. In the case presented, the patient’s symptoms—such as cough, fever, shortness of breath, and hemoptysis—initially pointed towards a diagnosis of Community-Acquired Pneumonia (CAP). However, several other conditions should be considered in the differential diagnosis when a patient presents with similar symptoms. These include:
1. Pneumonia
- Overlap: The most common misdiagnosis in this case, as pneumonia and PE often present with similar clinical features, such as cough, fever, shortness of breath, and wheezing. Chest X-ray findings such as consolidation or opacity can be suggestive of pneumonia, as seen in the initial radiological investigation.
- Distinguishing features: While pneumonia typically presents with localized consolidation on imaging, PE-related lung infarctions may show patchy consolidation or ground-glass opacities, indicating pulmonary infarction due to disrupted blood flow. In this case, the CTPA revealed a filling defect in the right pulmonary artery and signs of pulmonary infarction, which were more suggestive of PE rather than pneumonia.
2. Chronic Obstructive Pulmonary Disease (COPD) exacerbation: The patient’s background of smoking and sedentary lifestyle made this a plausible diagnosis.
3. Heart failure: The patient’s history of coronary artery disease raised concern for possible heart failure. In contrast to PE, heart failure typically presents with bilateral peripheral edema, orthopnea, and crackles on auscultation, particularly in the bases of the lungs. While this patient did have bilateral pedal edema, the presence of a filling defect on CTPA, along with the absence of heart failure-specific findings like pulmonary congestion on imaging, supported a diagnosis of PE.
4. Acute exacerbation of asthma: Wheezing was present in this case, the absence of a clear asthma history and the radiological findings of a filling defect rather than typical asthma-related hyperinflation or bronchial wall thickening favored a diagnosis of PE.
5. Deep Vein Thrombosis (DVT) with pulmonary embolism: DVT is a major risk factor for PE, and the two often occur together. The presence of pedal edema, especially when localized to one leg, may raise suspicion for DVT. This patient’s bilateral pedal edema, however, was not confined to one leg, which made DVT less likely as the primary diagnosis. Doppler ultrasound is the gold standard for diagnosing DVT. In this case, the Doppler ultrasound confirmed the presence of thrombosis in the lower limb, which further supported the diagnosis of PE. Additionally, the patient’s clinical presentation, including risk factors such as smoking and previous coronary artery disease, strengthened the suspicion of PE rather than isolated DVT.
- o Sepsis with pulmonary involvement: In this patient, despite elevated white blood cell count, the absence of systemic sepsis features and the specific findings on imaging (filling defect in the pulmonary arteries) directed the diagnosis toward PE rather than sepsis.
Inference on differential diagnosis
The differential diagnosis for a patient presenting with symptoms similar to pneumonia is broad and includes several life-threatening conditions, such as PE, which can masquerade as pneumonia. While the initial clinical and radiological findings pointed toward pneumonia, a high index of suspicion and further diagnostic testing, including CTPA and Doppler ultrasound, were crucial in identifying PE. Clinicians must maintain a broad differential diagnosis and use advanced imaging modalities to differentiate between these conditions, as prompt recognition of PE can significantly impact patient outcomes.
In clinical practice, pneumonia and PE can present with the same finding on Chest X-ray, resulting in a delay in the diagnosis of PE. Pneumonia and PE can occur in different scenarios [1].
- Firstly, infarction pneumonia, which occurs after PE.
- Secondly, CAP may coexist with underlying PE.
- Thirdly, septic pulmonary embolism is characterized by the presence of septic thrombi in the pulmonary circulation.
- Fourth, PE masquerading as pneumonia.
Pulmonary embolism can present with symptoms common to most respiratory conditions, often mimicking pneumonia. In this case, the initial diagnosis of CAP delayed the identification of PE. A high index of suspicion, especially in patients with risk factors such as smoking, obesity, and a history of cardiovascular disease, is critical for timely diagnosis. In the present case, all the risk factors are present.
Pulmonary embolism is a life-threatening condition that occurs when a dislodged blood clot usually from the deep lower limb vein, occludes the pulmonary circulation. It presents clinically with shortness of breath, pleuritic chest pain, coughing, orthopnoea, a history of painful swelling over the calf or thigh, wheezing, haemoptysis, and less commonly heart rhythm irregularities. It can also present with a syncopal attack or more devastatingly circulatory collapse [2].
In this elderly gentleman, we considered community-acquired pneumonia our first differential, due to his clinical presentation with fever, tachypnoea, cough, and raised leucocyte count. Pulmonary Embolism is often misdiagnosed as pneumonia because of similar clinical presentations. There have been cases of concomitant Pulmonary Embolism and Pneumonia in clinical practice. Several retrospective studies have already discussed pneumonia patients who have about 2–3-fold increased risk of venous thrombosis [3]. There are large-scale autopsy studies, including 1455 cases, which demonstrated concomitant presentation of PE and pneumonia, and out of 54 patients identified with anatomically major PE at autopsy, only 30% had correct ante-mortem diagnosis. However, the accuracy was more pronounced in postoperative patients. In 80% of cases in which lung scanning and pulmonary angiography were examined, there was an increased tendency for a correct diagnosis of PE. Among 21 patients with autopsy-proved major PE who also had pneumonia, PE was not diagnosed before death, indicating the importance of this discussion [4].
Pulmonary embolism was initially overlooked in our patient due to the predominance of symptoms pointing toward a chest infection as the primary diagnosis. Recognizing an underlying PE when pneumonia is diagnosed carries significant therapeutic importance, as timely initiation of anticoagulation therapy may be lifesaving.
To improve diagnostic accuracy, a prognostic model based on presenting symptoms and initial paraclinical findings could help identify patients at high risk for PE. These selected cases should then undergo computed tomography pulmonary angiography to confirm or exclude the diagnosis.
In situations where CTPA is contraindicated such as in patients with a contrast allergy, advanced heart failure, severe hypotension, inability to lie flat, or morbid obesity, or when CTPA findings are inconclusive, a ventilation-perfusion (V/Q) scan is recommended. While V/Q scanning has slightly lower sensitivity and specificity compared to CTPA, it remains a valuable diagnostic tool, as it can demonstrate impaired perfusion with normal ventilation, indicative of PE. This approach highlights the importance of integrating clinical, imaging, and risk assessment tools to avoid misdiagnosis and ensure appropriate management of PE [5].
Another modality to diagnose PE includes echocardiography and measuring the Echocardiography D-Dimer levels is usually done over the bedside, especially in conditions when other preferable modalities are not available or when the patient condition is too unstable to transfer, and it will show a nonspecific right ventricle (RV) strain in PE, such as enlarged RV size with reduced functionality, abnormal septal wall movement, and tricuspid regurgitation. Sometimes, RV thrombi can be visualised in echocardiography and usually signify a poor prognosis. The d-dimer level is usually measured when all other modalities are unavailable or in a condition where a patient with high risk but has normal CTPA finding. However, a normal D-dimer level does not rule out pulmonary embolism [6], as we see in our patient where the D-dimer level was not elevated.
The management of Pulmonary Embolism (PE) varies based on the patient’s hemodynamic stability.
- For stable patients: If the patient is stable and there are no contraindications to anticoagulant therapy, anticoagulation should be initiated and continued. If anticoagulation is contraindicated, an inferior vena cava (IVC) filter may be considered after confirming the diagnosis.
- For unstable patients:
- Initial steps: Begin resuscitation to stabilize the patient. If the patient becomes stable, start unfractionated heparin.
- Further evaluation: If instability persists, perform a 2D echocardiogram to assess for right ventricular (RV) strain.
- If there is no RV strain, investigate alternative causes for hemodynamic instability.
- If RV strain is present, initiate thrombolytic therapy unless contraindicated. Anticoagulation can be continued alongside thrombolysis.
- If thrombolytic therapy is contraindicated, surgical or catheter-directed embolectomy should be considered.
This structured approach ensures tailored management based on clinical status and available therapeutic options. In our case patient is stable and has no contraindication for anticoagulants so we started on anticoagulants.
In Payus, et al. case involved a patient with a history of multiple coronary interventions, ischemic heart disease, and partial immobilization due to degenerative spinal disease, with PE also presenting atypically, but without any history of trauma or DVT. In this case, the patient had no history of trauma, and the PE was suspected based on atypical pneumonia-like symptoms despite a normal D-dimer level. Additionally, the management approach was quite similar in both cases, with both patients receiving anticoagulation therapy. However, the detailed investigation in the second case included additional factors like echocardiography to rule out intracardiac issues and a more thorough assessment of cardiovascular health [7].
In a study, three cases presented with symptoms like fever, cough, chest pain, and shortness of breath, which initially seemed to be pneumonia. However, none showed consolidation as severe as in this case where the patient was suspected of having pneumonia due to similar symptoms but was later diagnosed with PE after further investigation. All cases were initially treated for pneumonia. However, as symptoms persisted or worsened (despite antibiotics), PE was suspected and confirmed [8].
This case report underscores the diagnostic challenges in managing a patient with pulmonary embolism (PE) presenting with symptoms mimicking severe pneumonia. The overlap in clinical, radiological, and laboratory findings between PE and pneumonia can lead to delays in identifying PE, a potentially life-threatening condition. While it is not suggested that all patients with similar presentations should be presumptively treated for PE, this case highlights the importance of maintaining a high index of suspicion for PE in the appropriate clinical context. A comprehensive clinical evaluation, supported by targeted imaging such as CT pulmonary angiography, is crucial for distinguishing PE from other pulmonary conditions. Early recognition and initiation of treatment are essential to improving patient outcomes and reducing the risk of complications.
Consent
Written informed consent was obtained from the patient to publish this case report.
- Sadeq AH, Farooqui MK, Sadiq Y. Pneumonia and concealed pulmonary embolism: A case report and literature review. J R Coll Physicians Edinb. 2022;52(2):142-146. Available from: https://doi.org/10.1177/14782715221103670
- Stein PD, Beemath A, Matta F, Weg JG, Yusen RD, Hales CA, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-9. Available from: https://doi.org/10.1016/j.amjmed.2007.03.024
- Rahman KK, Durgeshwar G, Mohapatra PR, Panigrahi MK, Mahanty S. Pulmonary infarct masquerading as community-acquired pneumonia in the COVID-19 scenario: A case report. World J Respirol. 2024;13(1):1-6. Available from: http://dx.doi.org/10.5320/wjr.v13.i1.1
- Goldhaber SZ, Hennekens CH, Evans DA, Newton EC, Godleski JJ. Factors associated with correct antemortem diagnosis of major pulmonary embolism. Am J Med. 1982;73:822-826. Available from: https://doi.org/10.1016/0002-9343(82)90764-1
- Anderson DR, Kahn SR, Rodger MA, Kovacs MJ, Morris T, Hirsch A, et al. Computed tomographic pulmonary angiography vs ventilation-perfusion lung scanning in patients with suspected pulmonary embolism: a randomized controlled trial. JAMA. 2007;298:2743. Available from: https://doi.org/10.1001/jama.298.23.2743
- Gibson NS, Sohne M, Gerdes VE, Nijkeuter M, Buller HR. The importance of clinical probability assessment in interpreting a normal d-dimer in patients with suspected pulmonary embolism. Chest. 2008;134(4):789–93. Available from: https://doi.org/10.1378/chest.08-0344
- Payus AO, Rajah R, Febriany DC, Mustafa N. Pulmonary Embolism Masquerading as Severe Pneumonia: A Case Report. Open Access Maced J Med Sci. 2019;7(3):396-399. Available from: https://doi.org/10.3889/oamjms.2019.114
- Evren H, Evren EÜ, Coşkun U. Pulmonary Embolism Mimicking Community-Acquired Pneumonia: A Case Series. Cyprus J Med Sci. 2019;4(1):60-62. Available from: https://cyprusjmedsci.com/articles/pulmonary-embolism-mimicking-community-acquired-pneumonia-a-case-series/doi/cjms.2019.752